Medication Related Osteonecrosis of the Jaw (MRONJ) is a rare multi-factorial condition characterized by non-healing exposed bone in patients with a history of an antiresorptive or antiangiogenic and no previous head and neck radiation. MRONJ is most often associated with invasive dental procedures such as tooth extraction, but can occasionally occur without or prior to dental intervention. Our treatment goals are general control of pain and infection as well as management of the bone necrosis and resorption. There are two general classes of medications responsible for MRONJ risk which are Bisphosphonates and RANK-ligand inhibitors. The Bisphosphonate medications to be concerned with are Aledronate (Fosamax), Risedronate (Actonel), Zoledronic Acid (Reclast), and Ibandronate (Boniva). Reclast and Boniva are IV, and generally higher risk for MRONJ than the per oral medications Fosamax and Actonel. All of these medications bind to bone, have a long half-life, and result in a reduced risk for vertebral fractures. The RANK-ligand Inhibitors to be concerned with are Denosumab (Prolia/Xgeva). The RANK-ligand inhibitors do not bind to bone, have a shorter half-life, result in a reduced risk for vertebral fractures, and are also used to treat metastatic bone disease. The risk for MRONJ with extraction while taking oral bisphosphonates is less than 1%. Extraction risk for MRONJ while taking Denosumab is as high as 1%. IV bisphosphonates present the highest risk after extraction with an MRONJ incidence as high as 15%. The risk for developing MRONJ with implants, endodontics, periodontal procedures or simply existing periodontal disease is not well documented but this certainly does happen. Disease in the mandible presents a higher risk as 75% of the cases present there versus 25% in the maxilla. Risk for MRONJ doubles in cancer patients taking IV bisphosphonates who also wear dentures. Other adjunctive risk factors are tobacco use, corticosteroid use, pre-existing inflammatory dental disease, and females over the age of 24. Clinical diagnosis usually involves exposed bone, or bone probed through a fistula for 8 weeks or more while having taken one of these medications in the absence of head and neck radiation. Osteoradionecrosis is another disease that presents very similarly with a different etiology and is another topic to be summarized in on its own.
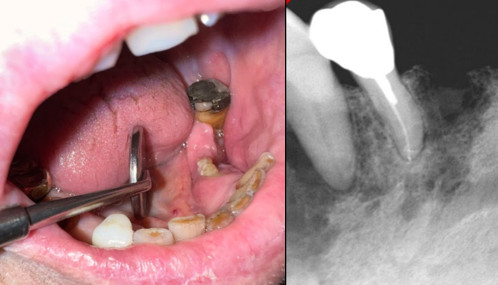
Our treatment goals will always include prevention, continued oncologic care, treatment of fragility risk factors but will clinically focus on preservation of quality of life including: education, reassurance, control of secondary infection and prevention of lesion extension. Preventive treatment modalities will include in some cases Chlorhexidine rinses BID, Chlorhexidine application with toothbrush, primary closure of extraction sockets, diabetes management, smoking cessation, holiday from the offending drug. A drug holiday may be 3-4 months, followed by 6-8 weeks to heal from the extraction or procedure. There are no biomarkers that are well validated to use as decision making adjuncts in diagnosis or treatment or MRONJ. CTX has been noted to be decreased in approximately 1/3 of patients taking bisphosphonate medications. Dentists can and should maintain involvement, optimize dental health, remind patients of the benefits of their anti-resorptive therapies, consider removal of crown in non-restorable teeth with endodontic treatment of roots in cancer patients on these medications, and provide chlorhexidine rinses to patients with exposed bone intraorally. OMS treatment will typically include staging the lesion, removal of a well formed bony sequestrum if present, debridement of exposed bone, systemic antibiotics and pain control. Promoting mucosalization of the exposed bone is the ultimate goal to be combined with maintenance of quality of life.







